Tests showed that cancer cells are less likely to spread if the white blood cells can be prevented from contacting the precursor cancer cells, suggesting that white blood cells – the immune cells – have the ability to promote disease by providing some kind of growth signal.
Interestingly, the chemical compound that acts as a draw between the two sets of cells was shown to be hydrogen peroxide – commonly used as a disinfectant or antiseptic, but also a harmless and natural by-product produced by the body’s metabolic process.
These dramatic findings, which are the result of a collaboration between academic colleagues in the UK and Italy (Institute of Molecular Oncology, Milan) are reported in the December edition of the prestigious online journal PLoS (Public Library of Science).
Describing the work, Paul Martin, Professor of Cell Biology at the University of Bristol’s Schools of Biochemistry and Physiology & Pharmacology, who supervised post-doc fellow Yi Feng in the research project, said: “By visualizing the earliest interactions between cancer cells and their host environment, we have shown that even from their earliest stages tumours don’t just avoid being destroyed by the immune system. Rather, they appear to court an immune response, co-opting the body’s innate immune system to aid and abet their growth.”
The team used several methods to express the human oncogene, or cancer-promoting white blood cell, HRAS, in early stage zebrafish embryos. The oncogene was labelled with different coloured fluorescent tags and engineered to be activated in a particular set of skin pigment cells, melanocytes.
Researchers monitored the first hours and days of development. As the embryo grew, some of the melanocytes were transformed by HRAS. Those transformed melanocytes were found to actively attract the innate immune cells. The researchers got the same results, after inserting HRAS into different mucous-secreting cells, and again when experimenting with a different oncogene, SRC.
Taking the tests one step further, the researchers found that a laser cut in the same region of the zebrafish larvae resulted in a very similar immune response. Early immune cells responded to the cut and to early cancer growth in a very similar manner - both wounds and tumour cells produced H2O2, and the researchers found that immune cells were drawn up the H2O2 gradient towards the cut or cancer, reinforcing a longstanding notion that cancers behave like a non-healing wound.
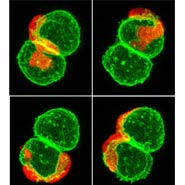
The researchers’ movies showed that white blood cells appeared to engulf cancerous cells in a bid to destroy them. However, other cells formed cytoplasmic tethers linking them to cancerous cells, and in some cases the cancerous cells appeared to drag white blood cells back when they started to leave the region.
In order to see whether the tumour was avoiding destruction or actually co-opting the immune cells, the researchers blocked the immune response in three different ways: they prevented the development of immune cells for the first three days after fertilization, and, separately, they used two different strategies to limit H2O2 production. In each case, immune cells failed to migrate to the cancer site. And each time, when the immune response was blocked, fewer cancer cells formed.
Prof Martin added: “Yi’s movies in Zebrafish larvae give us the first insight into how immune cells sense and then attempt to deal with the earliest stages of cancer. Now we can look closer to figure out why it is that immune cells seem to aid growth of these young cancer cells and figure out ways for guiding immune cells how better to search and destroy.”